In silico Delivery of ultrasound-sensitive microbubble for repairing the blood brain barrier
Introduction: The endothelial cells (ECs) in the blood brain barrier (BBB) are disrupted with age, genetic predisposition, or stroke and can lead to vascular cognitive impairment and dementia (VCID). Current treatments involve opening the BBB with high-frequency-ultrasound to deliver drugs, which alleviate the cognitive symptoms. However, we are proposing a unique delivery strategy that treats the fundamental cause of VCID by promoting EC growth. We previously experimentally released the gasotransmitter carbon monoxide (CO) from ruptured-microbubbles (MBs) and computationally demonstrated that the dose can benefit ECs. However, not all MBs are expected to rupture with ultrasound, and unruptured CO-loaded MBs can potentially reach the ECs at the BBB and provide benefits. Hence, we performed detailed particle tracking simulations that considered multiple driving forces that can impact MB movement.
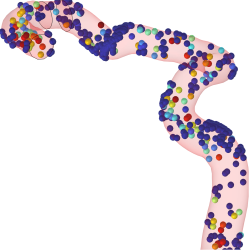
Material and Method: To understand the effects of ultrasound on MBs, we simulated steps in our overall delivery strategy (Figure-1A) in COMSOL Multiphysics®. We modeled MB movement in-silico with particle tracking, and the MBs were defined for perfluoropentane both in gas and liquid form. We defined a two part-model where we considered (1) ultrasound with acoustophoretic radiation as the driving force as well as drag and Brownian motion and (2) hemodynamics where the MBs movement was driven by pulsatile-blood-flow with buoyancy, Brownian motion and drag also considered. The ultrasound model considered acoustic streaming for pressure-induced blood flow. The impact of gravity, MBs size, and ruptures percentage were considered. Experimental studies were also performed to validate the response of MBs to ultrasound in our simulations.
Results and Conclusions: The in-silico model for hemodynamics with pulsatile blood flow yielded an average speed of 67.0 mm/s and resulted in ~8% of released particles that reach the ECs at the BBB after 8s (Figure-1D). The results also show that buoyancy and the direction of gravity can influence the percentage of MBs that reach the BBB, but only for the larger MBs (i.e., 3–5µm). Interestingly, ultrasound itself can cause MB movement (Figure-1C) in a different direction (i.e., the x direction). The in-silico model for ultrasound showed MB displacements (Figure-1B) within the region of application (i.e., 0.1-0.6 mm) that were comparable to experimental results (Figure-1E) with an 18 MHz transducer (i.e., 0.1-3.5 mm). We have also experimentally determined MBs velocity and rupture rate, including in response to different intensity (Figure-1F). These will be used for further comparison to the results from the simulation. Our ongoing computational studies involve understanding the impact of ultrasound frequency on MB movement and combining both ultrasound-induced and blood flow-induced MBs movement to determine the amount of MBs that can be available to ECs at the BBB. Overall, this study shows that CO can reach the ECs through CO-loaded MBs and different parameters will impact the provided dose. Further, this study shows that linking traditional ultrasound analysis with MB movement may be important. Finally, this approach shows potential as a treatment to restore the BBB, although further research is needed.
Acknowledgments This study was supported by a Brevard Foundation Medical Research Grant